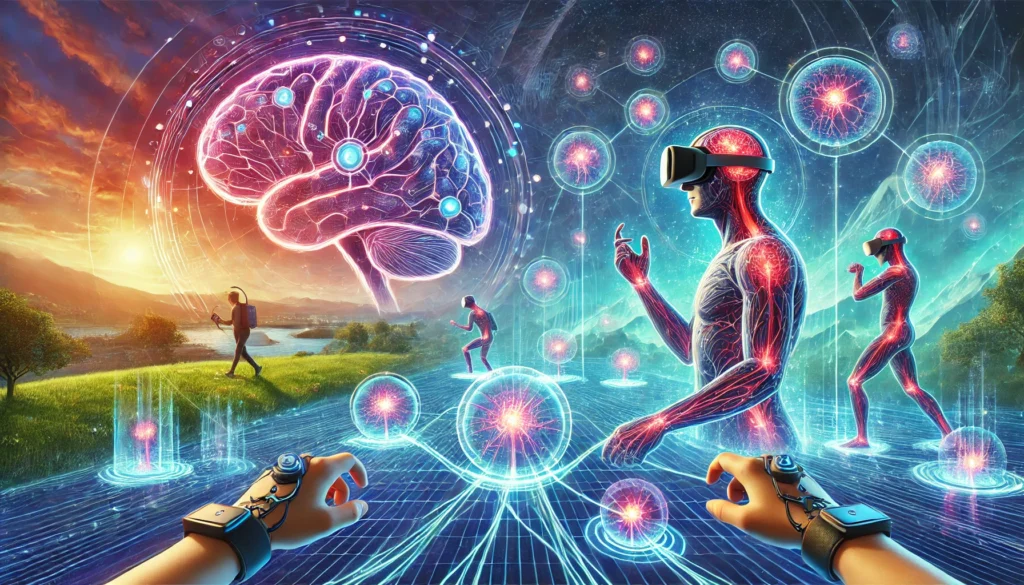
The fusion of virtual reality and cortical reorganization has emerged as a groundbreaking development in the field of neurorehabilitation. While virtual reality (VR) has been around for decades, its application in medical treatments, particularly in promoting cortical reorganization, is relatively new. As our understanding of the brain’s ability to reorganize itself grows, virtual reality and cortical reorganization have proven to be a powerful combination, helping patients recover from brain injuries, strokes, and various neurological conditions.
In this article, we will explore how virtual reality and cortical reorganization are revolutionizing rehabilitation, the science behind it, and the innovative technologies that are pushing the boundaries of brain recovery.
What is Virtual Reality (VR)?
Overview of Virtual Reality as an Immersive Experience
Virtual reality (VR) refers to an immersive digital environment that people can interact with using specialized equipment such as VR headsets, motion trackers, and haptic gloves. The experience provides real-time, three-dimensional visuals and sensory feedback, making users feel as though they are physically present in a virtual world. Initially popularized for gaming and entertainment, VR has evolved into a therapeutic tool with remarkable potential.
From Gaming to Therapeutics: The Evolution of VR
While VR was initially used for entertainment, its applications have expanded into fields like education, architecture, and healthcare. In particular, virtual reality and cortical reorganization have begun to intersect, creating a new avenue for patients recovering from neurological impairments. VR environments can simulate real-world activities and engage different parts of the brain, encouraging the rewiring of neural connections necessary for rehabilitation.
Knowing How the Cortical Reorganization Works
What is Cortical Reorganization?
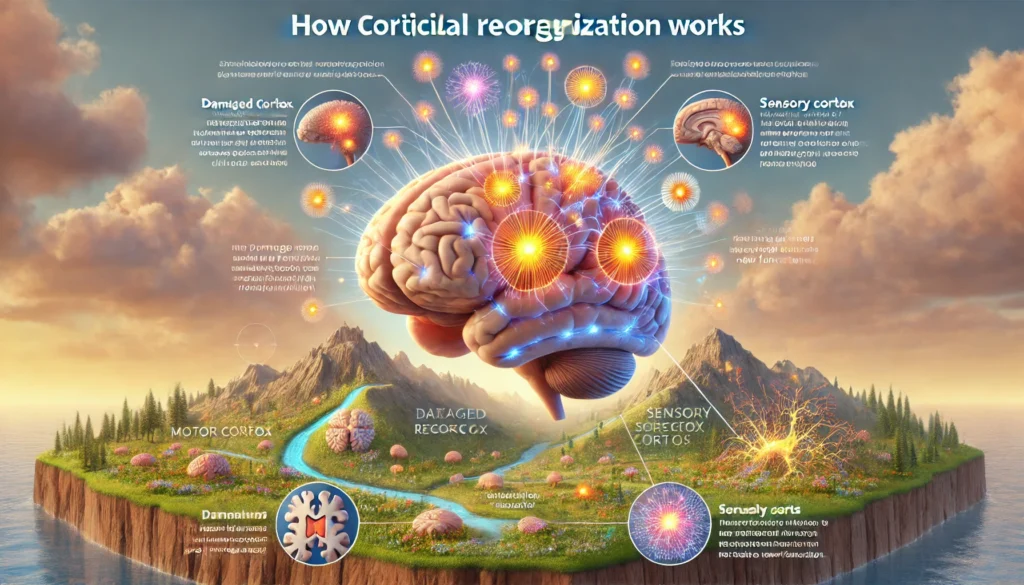
Cortical reorganization is the brain’s remarkable ability to change and adapt in response to injury, damage, or changes in sensory input. When a part of the brain is damaged (e.g., after a stroke), the brain “reorganizes” itself by reallocating functions to other undamaged regions. This process is known as neuroplasticity and is critical for recovery in many neurological conditions.
The Link Between Neural Plasticity and Cortical Reorganization
Neuroplasticity refers to the brain’s ability to form new neural connections and strengthen existing ones. It is the foundation of cortical reorganization. When a patient experiences an injury—whether it’s a stroke, traumatic brain injury, or spinal cord injury—neuroplasticity enables the brain to adapt by rerouting cognitive, sensory, and motor functions to other areas of the brain. Virtual reality and cortical reorganization are closely linked because VR provides the sensory input and stimulation necessary to activate and strengthen these new neural connections.
How Virtual Reality Promotes Cortical Reorganization
The Basics of VR in Rehabilitation
The immersive nature of VR provides a unique platform for rehabilitation. Using specially designed virtual environments, VR can simulate physical and cognitive tasks that patients may struggle to perform in the real world. By encouraging movement, cognitive challenges, and interaction with the environment, virtual reality and cortical reorganization come together to stimulate brain activity. These virtual tasks help the brain form new connections and promote healing in damaged areas.
How VR Stimulates Neuroplasticity
Virtual reality and cortical reorganization are a powerful combination because VR encourages patients to engage multiple senses—visual, auditory, and tactile—simultaneously. This multi-sensory stimulation enhances the process of neuroplasticity by providing the brain with the information it needs to build new connections and strengthen weak ones. As patients interact with virtual environments, their brains begin to “retrain” themselves, reorganizing sensory and motor functions that were previously lost due to injury or disease.
Examples of VR Applications in Cortical Reorganization
- Stroke Rehabilitation: VR allows stroke survivors to perform exercises that mimic real-life actions such as reaching, grasping, or walking. These simulated activities stimulate the motor cortex, helping patients regain movement and motor function.
- Spinal Cord Injury: VR provides a controlled environment where patients with spinal cord injuries can practice movement. This retrains the brain and encourages the neural pathways needed to restore physical abilities.
- Cognitive Rehabilitation: VR games and activities can improve cognitive functions like memory, problem-solving, and decision-making, which are often affected by brain injuries or neurodegenerative diseases.
- Phantom Limb Pain: For amputees suffering from phantom limb pain, VR is used to create visual feedback that helps retrain the sensory cortex and alleviate pain sensations associated with missing limbs.

Technological Innovations in VR for Cortical Reorganization
Advanced VR Hardware in Neurorehabilitation
The effectiveness of VR in rehabilitation has been greatly enhanced by advances in VR hardware. Modern devices like haptic gloves, motion-tracking suits, and VR headsets are being designed specifically for medical use. These devices allow for more precise movements and interactions, making virtual environments more realistic and engaging. By tracking the user’s movements and providing sensory feedback, this hardware supports the cortical reorganization process by stimulating specific brain regions.
AI Integration and Personalized Therapy
AI is playing a crucial role in the development of personalized VR therapies. Virtual reality and cortical reorganization can now be tailored to the needs of each patient. Using AI, VR systems adapt to the user’s progress, adjusting the difficulty level of exercises and tracking recovery. Machine learning algorithms help to monitor the patient’s performance and suggest modifications to enhance therapy. This dynamic and individualized approach makes VR rehabilitation more effective and engaging.
Real-Time Biofeedback and Brain-Computer Interfaces (BCIs)
Real-time biofeedback is another innovation that complements VR in promoting cortical reorganization. By monitoring physiological indicators such as heart rate, brainwaves, and muscle activity, VR systems can provide instant feedback, helping patients to optimize their rehabilitation efforts. Brain-computer interfaces (BCIs) allow for more direct communication between the brain and VR systems, further enhancing the brain’s ability to reorganize itself by promoting precise neural activation.
Clinical Applications and Success Stories
Stroke Rehabilitation
Several studies have shown that virtual reality and cortical reorganization are highly effective for stroke rehabilitation. For example, one study demonstrated that stroke survivors using VR showed significant improvements in motor function and the ability to perform daily activities. By simulating movement and providing real-time feedback, VR helps patients “relearn” lost motor skills, fostering recovery through cortical reorganization.
Neurodegenerative Diseases
Virtual reality and cortical reorganization also have promising applications for neurodegenerative diseases such as Alzheimer’s and Parkinson’s. For patients with these conditions, VR is used to stimulate the brain and slow cognitive decline. VR-based exercises help improve memory, coordination, and overall brain function by promoting neuroplasticity.
Spinal Cord Injury Rehabilitation
For patients recovering from spinal cord injuries, VR has shown significant success in improving physical rehabilitation. VR helps retrain the brain by providing virtual experiences of movement, making it possible for patients to practice motor skills and regain functionality in ways that were previously unimaginable.
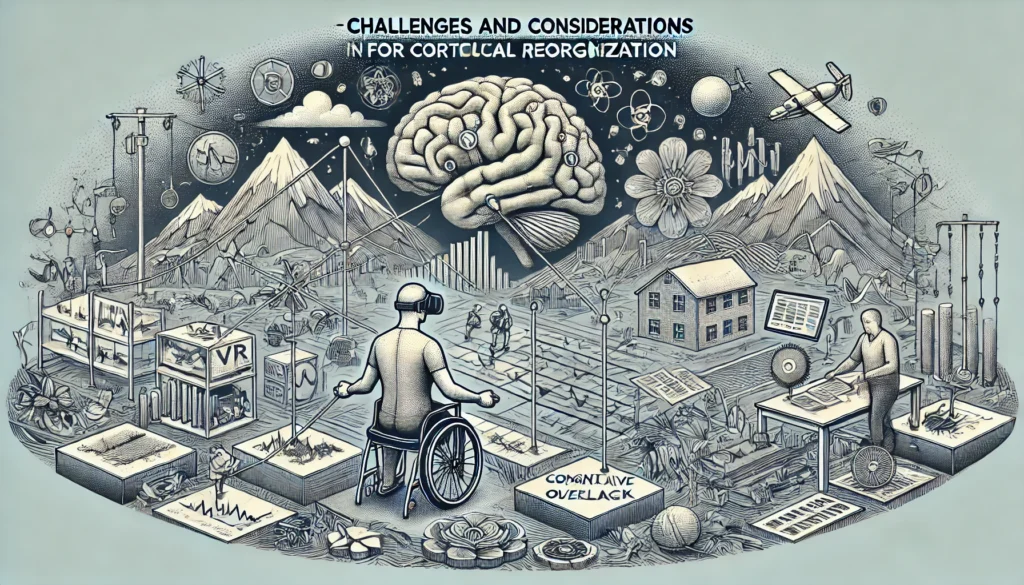
Challenges and Considerations in VR for Cortical Reorganization
Limitations of Current VR Technology
While virtual reality and cortical reorganization have immense potential, there are some limitations. The cost of high-quality VR hardware can be prohibitive, and many patients may not have access to the specialized devices needed for treatment. Moreover, there is still a gap between commercially available VR systems and those used in medical rehabilitation, with medical-grade VR requiring greater precision and customizability.
Personalized Therapy: A Key Challenge
Each patient’s recovery process is unique, which means VR therapies need to be personalized. Not all patients respond in the same way to virtual reality and cortical reorganization. Tailoring VR environments to each patient’s needs can be challenging, but advancements in AI and machine learning are helping to address this issue by creating adaptive, personalized VR experiences.
Ethical and Safety Considerations
VR technology is still evolving, and there are potential risks to consider, particularly for vulnerable populations. Issues such as motion sickness, cognitive overload, and excessive screen time may pose challenges for some patients. Ensuring the safety and comfort of patients is crucial, and ongoing research is needed to fully assess the long-term effects of VR in neurorehabilitation.
FAQs
1. How does virtual reality promote cortical reorganization?
VR helps promote cortical reorganization by stimulating the brain through multi-sensory environments. The immersive nature of VR engages the motor, sensory, and cognitive regions of the brain, facilitating new neural connections and enhancing recovery.
2. Is VR effective for stroke rehabilitation?
Yes, VR has proven to be highly effective in stroke rehabilitation. By simulating real-world activities, it helps stroke survivors practice movements, improve motor function, and accelerate cortical reorganization in the affected brain regions.
3. Can VR be used to treat phantom limb pain?
Yes, VR is an effective treatment for phantom limb pain. By creating visual feedback for amputees, VR helps retrain the brain’s sensory cortex, reducing pain and aiding in cortical reorganization.
4. What neurological conditions can benefit from VR therapy?
Conditions like stroke, spinal cord injuries, brain trauma, Alzheimer’s, and Parkinson’s disease can all benefit from virtual reality and cortical reorganization. VR promotes neural plasticity, helping patients recover motor and cognitive functions.
5. What does the future hold for VR in brain rehabilitation?
The future of VR in brain rehabilitation looks promising, with the integration of AI, real-time biofeedback, and personalized therapies. As technology continues to advance, virtual reality and cortical reorganization will likely become even more effective, enabling faster and more comprehensive recovery.
Conclusion
Virtual reality and cortical reorganization are at the forefront of neurorehabilitation, offering hope for individuals recovering from neurological conditions. By leveraging immersive, interactive environments, VR stimulates the brain’s natural healing processes, encouraging neuroplasticity and promoting functional recovery. With continued innovation, virtual reality and cortical reorganization will likely transform rehabilitation, providing patients with more effective and personalized treatment options.